A large number of fraudulent activities in healthcare, increasing number of patients seeking health insurance, high returns on investment, and the rising number of pharmacy claims-related frauds. However, the dearth of skilled personnel is expected to restrain the growth of this market.
[176 Pages Report] Fraud analytics is the efficient use of data analytics and related business insights developed through statistical, quantitative, predictive, comparative, cognitive, and other emerging applied analytical models for detecting and preventing healthcare fraud.
The healthcare industry has been witnessing a number of cases of frauds, done by patients, doctors, physicians, and other medical specialists. Many healthcare providers and specialists have been observed to be engaged in fraudulent activities, for the sake of profit. In the healthcare sector, fraudulent activities done by patients include the fraudulent procurement of sickness certificates, prescription fraud, and evasion of medical charges.
Download PDF Brochure @ https://www.marketsandmarkets.com/pdfdownloadNew.asp?id=221837663
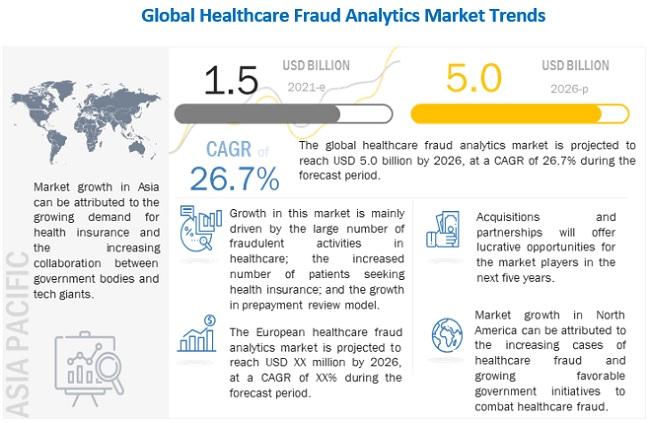
Emerging markets such as Asia promise significant growth in health insurance coverage, mainly due to increasing government initiatives, rising government and private investments for promoting medical insurance, and growing income levels. This growth is aided by the increasing affordability of health insurance for the middle class in this region and the rising awareness regarding the benefits of health insurance.
The healthcare industry is changing at an incredible rate, and one of the major contributors to this change is the increasing popularity of healthcare communication through social media.
This vast network of healthcare influencers, leaders, patients, providers, organizations, and governmental entities creates a massive amount of healthcare data on a regular basis. This data, if segregated, segmented, and analyzed in a meaningful way, can offer incredible value for improving treatment efficiencies and health outcomes. This has created a demand for data aggregation and analytical tools and thus acts as an opportunity for the healthcare fraud analytics market during the forecast period.
The increasing number of patients seeking health insurance, the rising number of fraudulent claims, and the growing adoption of the prepayment review model are expected to drive the growth of this segment in the coming years.
The prominent players in Healthcare Fraud Analytics Market are IBM Corporation (US), Optum, Inc. (US), Cotiviti, Inc. (US), Change Healthcare (US), Fair Isaac Corporation (US), SAS Institute Inc. (US), EXLService Holdings, Inc. (US), Wipro Limited (India), Conduent, Incorporated (US), CGI Inc. (Canada), HCL Technologies Limited (India), Qlarant, Inc. (US), DXC Technology (US), Northrop Grumman Corporation (US).
